
What is a Rectocele?
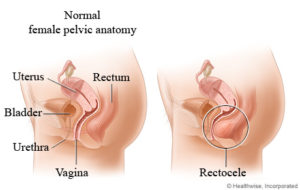
Normal anatomy and a rectocele
A rectocele is a type of pelvic organ prolapse. It happens when the supporting ligaments and muscles weaken in the pelvic floor. Other names for a rectocele are a posterior vaginal wall prolapse or proctocele.
Childbirth, age, and a range of other factors can cause the normally tough, fibrous, sheet-like divider between the rectum and vagina to weaken.
A bulge may protrude as a hernia into the back of the vagina during a time of straining, such as a bowel movement.
A rectocele can lead to constipation and discomfort, but if it is small, there may be no symptoms.
Most people can treat a rectocele at home, but a severe case may need surgery.
NONSURGICAL TREATMENT
The following tips can help prevent a rectocele from developing, and — if a rectocele is already present — stop symptoms from getting worse.
- Pelvic floor exercises, such as Kegel exercises, can strengthen the pelvic floor muscles.
- Drinking plenty of fluids and eating high-fiber foods can reduce constipation.
- Avoiding any type of heavy lifting can also prevent a worsening of symptoms.
- Getting treatment for prolonged coughing can reduce strain on the pelvic floor muscles.
- Losing weight may be advisable if a person has obesity or excess weight.
- Straining for a long time when defecating can make the problem worse. Avoiding constipation can help prevent this.
Medications
The doctor may prescribe:
stool softeners to ease constipation
hormone replacement therapy (HRT) for use after menopause.
a vaginal pessary — a plastic or rubber round disk inserted into the vagina — to support the protruding tissues
SURGERY
there are interventions for different kinds of pelvic organ prolapse include:
- sacral colpopexy
- sacrospinous colpopexy
- uterosacral colpopexy
- transvaginal mesh (PLEASE NOTE THAT TRANSVAGINAL MESH IS NO LONGER ROUTINELY PERFORMED IN THE UNITED STATES. THIS OPTION IS OUT-OF-DATE)
The surgeon can remove the stretched or damaged tissue. Sometimes they may use a mesh inlay to reinforce the wall between the vagina and the rectum.
The technique can vary from open surgery to a minimally invasive procedure. In some cases, a surgeon will repair the damaged tissue, usually through an incision in the vagina.
The gynecologist will discuss the options with the patient, and the choice is likely to depend on the extent of prolapse, and the individual’s situation, including age, general health and whether or not they want to have more children.
To learn more, visit:
https://www.medicalnewstoday.com/articles/189696
